Lucas’s Minimally Invasive Epilepsy Surgery Story
Nov 19, 2019Ypsilanti Infant Successfully Treated with Minimally Invasive Epilepsy Surgery
 Despite developing gestational diabetes that was controlled through diet, Jessica of Ypsilanti, Michigan was thankful to welcome her second child into the family. Lucas was born and appeared to be healthy, but a few weeks after his birth, there were signs that all was not right.
Despite developing gestational diabetes that was controlled through diet, Jessica of Ypsilanti, Michigan was thankful to welcome her second child into the family. Lucas was born and appeared to be healthy, but a few weeks after his birth, there were signs that all was not right.
“Lucas was about 3 weeks old, and he turned blue when I was nursing him. He seemed to be o.k. after that and I thought it might have been because he was choking from the milk. The same thing happened shortly after that when I was changing his diaper, and I knew something was wrong since he was not eating during that time,” Jessica says.
Lucas was seen at a local hospital where an MRI revealed that he had two serious conditions affecting the right side of his brain causing seizures. The first was polymicrogyria, an abnormal brain development where the surface of the brain has many ridges or folds. The second condition was hemimegalencephaly, where one side of the brain, is abnormally larger than the other. The enlarged brain tissue causes frequent seizures, often associated with cognitive or behavioral disabilities.
Lucas was put on several anti-seizure medications, but his seizures continued.
 “It was very distressing because tests revealed he appeared to be having 20 or more seizures in three days despite the medical treatment,” Jessica says.
“It was very distressing because tests revealed he appeared to be having 20 or more seizures in three days despite the medical treatment,” Jessica says.
Surgery was recommended to stop the seizures. Jessica and her husband researched top hospitals within and outside of the state to determine the best course of treatment. Neurosurgeons were hesitant to operate on Lucas because of the high risk of standard hemispherectomy at his young age. They wanted to wait till he was older. But waiting was not an option, since it results in poorer developmental outcomes. Finally, the parents met with Sandeep Sood, MD, co-director of the Epilepsy Surgery Program at Children’s Hospital of Michigan and a pioneer in minimally invasive endoscopic hemispherotomy which was developed and started at the Children’s Hospital of Michigan by Dr. Sood. He felt confident that the minimally invasive endoscopic hemispherotomy was the best option for Lucas. At his young age, it carried the least risk because of a smaller incision and low blood loss. In 2015, the first series of his experience was published in Journal of Neurosurgery Pediatrics, the Official Journal of the American Association of Neurological Surgeons. The effectiveness of his endoscopy-based epilepsy surgery techniques was subsequently highlighted in a systematic review article published in Epilepsia, the Official Journal of the International League Against Epilepsy. Dr. Sood and his colleagues recently reported the results of open hemispherectomy and endoscopic hemispherotomy performed in 86 patients at Children’s Hospital of Michigan in Child Nervous System, the official journal of the International Society for Pediatric Neurosurgery. The data suggested that 90% of patients with a unilateral focus successfully achieved seizure control following either hemispherectomy or hemispherotomy.
“Dr. Sood had the most experience with the minimally invasive surgery option, and we immediately felt comfortable in our decision when we met him. He was confident, assuring and experienced, and it was important for us that there was an entire dedicated, experienced team including pediatric neurologists and nurses that would be managing his treatment and care,” Jessica explains.
Lucas was 5 months old when the minimally invasive surgical procedure took place. Dr. Sood worked with a team of pediatric epilepsy experts on staff including Director of Neurodiagnostics Eishi Asano, MD, PhD and Staff Pediatric Neurologist, Aimee Luat, MD.
Dr. Asano explains that before making the surgical decision, the multidisciplinary epilepsy management team evaluated Lucas’s seizure activity using video-EEG monitoring and found that his right hemisphere generated seizures every few hours despite the intense medical treatment initiated before the admission.
“The brain mapping using diffusion-weighted imaging tractography showed that the motor pathway in the right hemisphere had been already severely thinned out, whereas that in the left appeared well-formed. Indeed, Lucas’s left hand and leg supported by the right motor pathway were less active compared to those on the other side. We realized that frequent seizure activity arising from the right-side seizure focus and traveling to the healthy left-hemispheric brain would eventually hinder his development. We were aware that the chance of seizure control would range less than 10% with continued medical therapy but around 90% with epilepsy surgery in his case. We also expected that right-sided hemispherotomy would protect the left hemisphere from the unwanted effect of traveling seizure activity, facilitate the functional reorganization of the left hemisphere, and optimize the development of his cognitive function,” he says.

Dr. Sood explains that unlike traditional, anatomical or functional hemispherotomy, endoscopic hemispherotomy is done through a small incision and results in minimal blood loss. It is ideal for very young children who cannot withstand the risk of the traditional epilepsy operation.
“Recently, we successfully performed this operation on a child who weighed only 8 pounds and like Lucas, was turned away from other centers because of a high risk of traditional operation,” says Dr. Sood.
Although Lucas did undergo another procedure after his initial surgery including one to eliminate a bump on his head due to fluid in the incision, Jessica is happy to report that Lucas who is now 1, has been seizure free for the past several months.
Dr. Luat says that he will be required to take anti-seizure medication for at least 2 years and the decision to wean will be guided clinically and by EEG monitoring.
“Currently, Lucas is on his way to a full recovery and is making progress with his development. At the age of 12 months, he has started standing up with support, able to make some words and is very social and interactive,” she says.
Jessica and her husband are very appreciative of the entire Children’s Hospital of Michigan epilepsy team including members of the neurology, neurosurgery, and nursing staff that worked so well together to manage her son’s care.
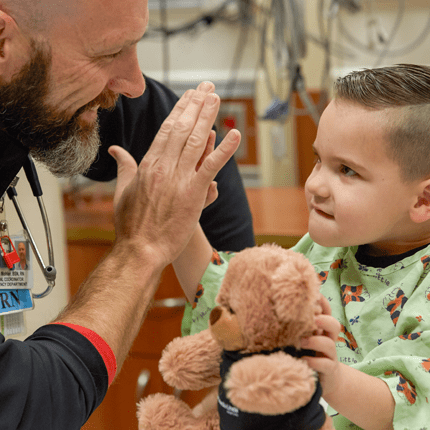
“This was a very hard journey, but we are so amazed at how well Lucas is doing. He is a few months behind developmentally but is catching up quickly and is a very happy baby. It was a terrifying process, but we are so thankful to the nurses and doctors who were so caring and treated Lucas like their own child. It was well worth it,” Jessica says.